By Bogdana Rakova, Research Fellow at Partnership on AI, Data Scientist at Accenture.
This summary introduces the results from preliminary analysis of the CORD-19 research dataset and aims to investigate the ethical and social science considerations regarding pandemic outbreak response efforts. In particular, we identify the research articles in the dataset which discuss the potential barriers and enablers for the uptake of public health measures for prevention and control.
We also identify articles discussing the implications of public health measures to vulnerable groups such as front-line care providers, elderly, homeless communities, gig workers, and others. We hope that these findings are helpful in highlighting how others have been able to address social and ethical considerations during critical pandemic response efforts. In this way we aim to provide more resources to policy-makers, decision-makers, ethicists who might be part of a hospital ethics committee, or other individuals who need to navigate similar difficult decisions.
Findings
- The scientific literature has put a lot of attention into studying the social and ethical concerns of public information campaigns, restrictions on internal movement such as city lockdown and quarantine, healthcare interventions and vaccines, and recently the considerations regarding contact tracing.
- Much less attention has historically been given to the implications of public health measures deployed in certain sociocultural and socioeconomic contexts.
On March 16th, the White House published a call to action to the tech community on a new machine readable dataset of scholarly literature about COVID-19, SARS-CoV-2, and the Coronavirus group (CORD-19). The CORD-19 dataset is a free resource of over 52,000 scholarly articles, including over 41,000 with full text. The dataset has been made available by the Allen Institute for AI, Chan Zuckerberg Initiative (CZI), Georgetown University’s Center for Security and Emerging Technology (CSET), Microsoft, and the National Library of Medicine (NLM) at the National Institutes of Health.
AI research has evolved natural language processing (NLP) and natural language understanding (NLU) algorithms that power many of the conversational AI systems in use today. Many of them are rule-based, for example the queries a user asks to a chatbot are matched to predefined rules, the algorithm is then able to extract the intent of the query and use that information to return a satisfying answer. More complex algorithms utilizing Deep Learning and other methods have shown better results, however, current state-of-the-art systems are still a long way from engaging in truly natural everyday conversations with humans. The NLP/NLU challenges we faced while working on the CORD-19 dataset were similar but also much simpler than the challenges in working with free-form multi-turn language data. For example, we had to consider what techniques could allow us to address common-sense reasoning for understanding concepts as well as context modeling for relating past concepts.
The Oxford COVID-19 Government Response Tracker (OxCGRT) project by the Blavatnik School of Government, University of Oxford, provides systematic updates on the policy actions taken in response to the crisis. The data is continuously updated and publicly available. The OxCGRT policy response metrics framework includes 13 indicators listed below (read the OxCGRT working white paper here). Through our research analysis of the CORD-19 corpus, we aim to further identify the social and ethical concerns related to each of these indicators.
What are the barriers and enablers (BLUE) for the uptake of public health measures and their implications (RED) given the variation in policy responses?
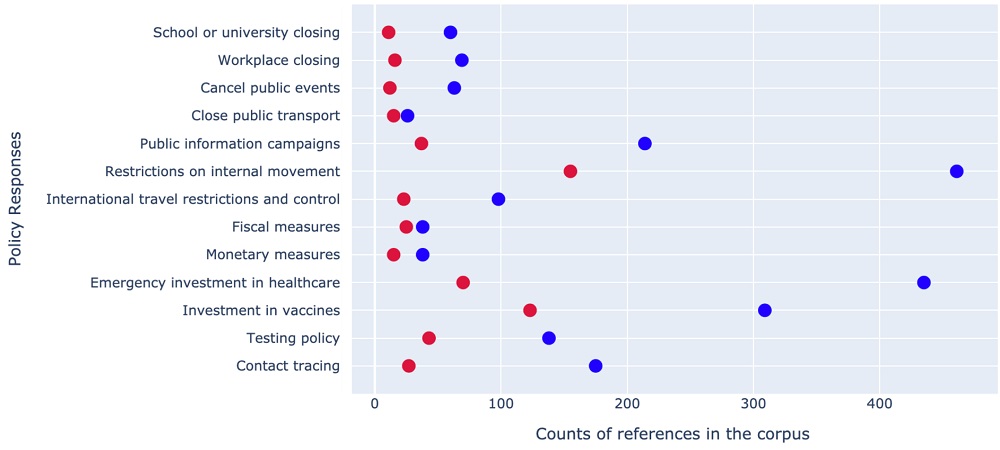
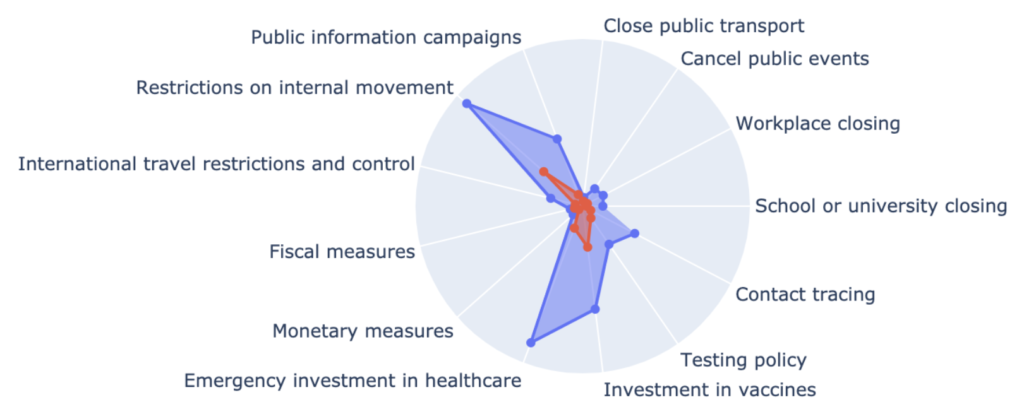
The data vizualization shows the number of CORD-19 references to each of the indicators where the similarity between conepts discussed in the dataset and the OxCGRT indicators was calculated using a Deep Learning model – Tensorflow’s Universal Sentence Encoder model.
In what follows, we highlight the top research references that were found to discuss the social and ethical considerations of each individual policy response indicator. Learn more about the technical details and explore the source code within our interactive notebook in the Kaggle platform.
School closing
Wilcox, B. A., Gubler, D. J., & Pizer, H. F. (2008). Urbanization and the social ecology of emerging infectious diseases. In The social ecology of infectious diseases (pp. 113-137). Academic Press.
Jefferson, T., Foxlee, R., Del Mar, C., Dooley, L., Ferroni, E., Hewak, B., … & Rivetti, A. (2008). Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. Bmj, 336(7635), 77-80.
Hou, J., Wang, Z., Liu, X., Luo, Y., Sabharwal, S., Wang, N., & Meng, Q. (2018). Public health education at China’s higher education institutions: a time-series analysis from 1998 to 2012. BMC public health, 18(1), 679. https://doi.org/10.1186/s12889-018-5605-4
Workplace closing
Hsiang, S., Allen, D., Annan-Phan, S., Bell, K., Bolliger, I., Chong, T., … & Lau, P. (2020). The Effect of Large-Scale Anti-Contagion Policies on the Coronavirus (COVID-19) Pandemic. medRxiv.
Kok, G., Jonkers, R., Gelissen, R., Meertens, R., Schaalma, H., & de Zwart, O. (2010). Behavioural intentions in response to an influenza pandemic. BMC public health, 10, 174. https://doi.org/10.1186/1471-2458-10-174
Schwartz, J., & Yen, M. Y. (2017). Toward a collaborative model of pandemic preparedness and response: Taiwan’s changing approach to pandemics. Journal of Microbiology, Immunology and Infection, 50(2), 125-132.
Blake, K. D., Blendon, R. J., & Viswanath, K. (2010). Employment and compliance with pandemic influenza mitigation recommendations. Emerging infectious diseases, 16(2), 212–218. https://doi.org/10.3201/eid1602.090638
Cancel public events
Herida, M., Dervaux, B., & Desenclos, J. C. (2016). Economic Evaluations of Public Health Surveillance Systems: a Systematic Review. European journal of public health, 26(4), 674–680. https://doi.org/10.1093/eurpub/ckv250
Schilling, S., Maltezou, H. C., Fusco, F. M., De Iaco, G., Brodt, H. R., Bannister, B., … & Ippolito, G. (2013). Transportation capacity for patients with highly infectious diseases in Europe: A survey in 16 nations. Clinical Microbiology and Infection.
Zhang, X. S., Pebody, R., Charlett, A., de Angelis, D., Birrell, P., Kang, H., Baguelin, M., & Choi, Y. H. (2017). Estimating and modelling the transmissibility of Middle East Respiratory Syndrome CoronaVirus during the 2015 outbreak in the Republic of Korea. Influenza and other respiratory viruses, 11(5), 434–444. https://doi.org/10.1111/irv.12467
McCloskey, B., Zumla, A., Ippolito, G., Blumberg, L., Arbon, P., Cicero, A., … & Group, M. G. E. (2020). Mass gathering events and reducing further global spread of COVID-19: a political and public health dilemma. Lancet (London, England), 395(10230), 1096.
Close public transport
Lin, S., Huang, J., He, Z., & Zhan, D. (2020). Which Measures are Effective in Containing COVID-19? Empirical Research Based on Prevention and Control Cases in China. medRxiv.
Schilling, S., Maltezou, H. C., Fusco, F. M., De Iaco, G., Brodt, H. R., Bannister, B., … & Ippolito, G. (2013). Transportation capacity for patients with highly infectious diseases in Europe: A survey in 16 nations. Clinical Microbiology and Infection.
Boas, T. C., & Hidalgo, F. D. (2019). Electoral incentives to combat mosquito-borne illnesses: Experimental evidence from Brazil. World Development, 113, 89-99.
Lee L. M. (2013). Health Information in the Background: Justifying Public Health Surveillance Without Patient Consent. Emerging Pervasive Information and Communication Technologies (PICT): Ethical Challenges, Opportunities and Safeguards, 11, 39–53. https://doi.org/10.1007/978-94-007-6833-8_3
Public info campaigns
Enanoria, W. T., Liu, F., Zipprich, J., Harriman, K., Ackley, S., Blumberg, S., Worden, L., & Porco, T. C. (2016). The Effect of Contact Investigations and Public Health Interventions in the Control and Prevention of Measles Transmission: A Simulation Study. PloS one, 11(12), e0167160. https://doi.org/10.1371/journal.pone.0167160
Peng, L., Yang, W., Zhang, D., Zhuge, C., & Hong, L. (2020). Epidemic analysis of COVID-19 in China by dynamical modeling. arXiv preprint arXiv:2002.06563.
Gable, L., & Hodge, J. G., Jr (2008). Public Health Law and Biological Terrorism. Beyond Anthrax: The Weaponization of Infectious Diseases, 239–252. https://doi.org/10.1007/978-1-59745-326-4_12
Ambe, J. R., & Kombe, F. K. (2019). Context and Ethical Challenges During the Ebola Outbreak in West Africa. Socio-cultural Dimensions of Emerging Infectious Diseases in Africa: An Indigenous Response to Deadly Epidemics, 191–202. https://doi.org/10.1007/978-3-030-17474-3_14
Shao, P. (2020). Impact of city and residential unit lockdowns on prevention and control of COVID-19. medRxiv.
Restrictions on internal movement
Enanoria, W. T., Liu, F., Zipprich, J., Harriman, K., Ackley, S., Blumberg, S., Worden, L., & Porco, T. C. (2016). The Effect of Contact Investigations and Public Health Interventions in the Control and Prevention of Measles Transmission: A Simulation Study. PloS one, 11(12), e0167160. https://doi.org/10.1371/journal.pone.0167160
Peng, L., Yang, W., Zhang, D., Zhuge, C., & Hong, L. (2020). Epidemic analysis of COVID-19 in China by dynamical modeling. arXiv preprint arXiv:2002.06563.
Gable, L., & Hodge, J. G., Jr (2008). Public Health Law and Biological Terrorism. Beyond Anthrax: The Weaponization of Infectious Diseases, 239–252. https://doi.org/10.1007/978-1-59745-326-4_12
International air travel controls
Findlater, A., & Bogoch, I. I. (2018). Human mobility and the global spread of infectious diseases: a focus on air travel. Trends in parasitology, 34(9), 772-783.
Rodriguez, J., Acuna, J. M., Uratani, J. M., & Paton, M. (2020). A mechanistic population balance model to evaluate the impact of interventions on infectious disease outbreaks: Case for COVID19. medRxiv.
Uribe-Sánchez, A., & Savachkin, A. (2011). Predictive and Reactive Distribution of Vaccines and Antivirals during Cross-Regional Pandemic Outbreaks. Influenza research and treatment, 2011, 579597. https://doi.org/10.1155/2011/579597
Fiscal measures / What economic stimulus policies are adopted?
Yip, P., Chen, M., So, B. K., Lam, K. F., & Wat, K. P. (2020). Optimal Strategies for Reducing Number of People in the Social Security System. International journal of environmental research and public health, 17(4), 1305. https://doi.org/10.3390/ijerph17041305
Daemmrich A. (2013). The political economy of healthcare reform in China: negotiating public and private. SpringerPlus, 2, 448. https://doi.org/10.1186/2193-1801-2-448
Yang, P., Qi, J., Zhang, S., Bi, G., Wang, X., Yang, Y., … & Mao, X. (2020). Feasibility of Controlling COVID-19 Outbreaks in the UK by Rolling Interventions. medRxiv.
Aboagye-Sarfo, P., Mueller, U., & Cross, J. (2015). The impact of the activities of Ghana AIDS Commission on new HIV infections in Ghana: An intervention time series analysis. HIV & AIDS Review, 14(4), 97-103.
Monetary measures / What monetary policy interventions are adopted?
Maharaj, S., & Kleczkowski, A. (2012). Controlling epidemic spread by social distancing: do it well or not at all. BMC public health, 12, 679. https://doi.org/10.1186/1471-2458-12-679
Lo, H. W. A., Su, C. Y., & Chou, F. H. C. (2012). Disaster psychiatry in Taiwan: a comprehensive review. Journal of Experimental & Clinical Medicine, 4(2), 77-81.
Hernandez, M., Milechin, L. E., Davis, S. K., DeLaura, R., Claypool, K. T., & Swiston, A. (2020). The Impact of Host-Based Early Warning on Disease Outbreaks. medRxiv.
Race, J. D., Nichols, C., & Blumenthal, S. R. (2016). Chemical, Biological, Radiological, and Nuclear Quarantine. Ciottone’s Disaster Medicine, 504.
Emergency investment in health care
Herida, M., Dervaux, B., & Desenclos, J. C. (2016). Economic Evaluations of Public Health Surveillance Systems: a Systematic Review. European journal of public health, 26(4), 674–680. https://doi.org/10.1093/eurpub/ckv250
Lim, S., Closson, T., Howard, G., & Gardam, M. (2004). Collateral damage: the unforeseen effects of emergency outbreak policies. The Lancet Infectious Diseases, 4(11), 697-703.
McLaughlin, M. M., Lee, M. C., Hall, B. J., Bulterys, M., Ling, L., & Tucker, J. D. (2014). Improving health services for African migrants in China: A health diplomacy perspective. Global public health, 9(5), 579-589.
Yang, L., Sun, L., Wen, L., Zhang, H., Li, C., Hanson, K., & Fang, H. (2016). Financing strategies to improve essential public health equalization and its effects in China. International journal for equity in health, 15(1), 194. https://doi.org/10.1186/s12939-016-0482-x
Investment in vaccines
Chan, S. S., Leung, D. Y., Leung, A. Y., Lam, C., Hung, I., Chu, D., … & Lam, T. H. (2015). A nurse-delivered brief health education intervention to improve pneumococcal vaccination rate among older patients with chronic diseases: a cluster randomized controlled trial. International journal of nursing studies, 52(1), 317-324.
Uribe-Sánchez, A., & Savachkin, A. (2011). Predictive and Reactive Distribution of Vaccines and Antivirals during Cross-Regional Pandemic Outbreaks. Influenza research and treatment, 2011, 579597. https://doi.org/10.1155/2011/579597
Tulchinsky, T. H. (2018). Maurice Hilleman: Creator of Vaccines That Changed the World. Case Studies in Public Health, 443.
Testing policy
Liu, C., Zhao, J., Liu, G., Gao, Y., & Gao, X. (2020). D2EA: Depict the Epidemic Picture of COVID-19. Journal of Shanghai Jiaotong University (science), 25(2), 165–176. https://doi.org/10.1007/s12204-020-2170-7
Wabe, N., Li, L., Lindeman, R., Yimsung, R., Dahm, M. R., Clezy, K., McLennan, S., Westbrook, J., & Georgiou, A. (2019). The impact of rapid molecular diagnostic testing for respiratory viruses on outcomes for emergency department patients. The Medical journal of Australia, 210(7), 316–320. https://doi.org/10.5694/mja2.50049
Contact tracing
Arita, I., Nakane, M., & Nakano, T. (2008). Surveillance of disease: Overview. International encyclopedia of public health, 275.
Neill, D. B., & Soetebier, K. A. (2011). International society for disease surveillance conference 2011: building the future of public health surveillance. Emerging health threats journal, 4, 11702. https://doi.org/10.3402/ehtj.v4i0.11702
Hellewell, J., Abbott, S., Gimma, A., Bosse, N. I., Jarvis, C. I., Russell, T. W., … & Flasche, S. (2020). Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. The Lancet Global Health.
Kwok, K. O., Cowling, B., Wei, V., Riley, S., & Read, J. M. (2018). Temporal variation of human encounters and the number of locations in which they occur: a longitudinal study of Hong Kong residents. Journal of the Royal Society, Interface, 15(138), 20170838. https://doi.org/10.1098/rsif.2017.0838
Moyen, N., Ahmed, G., Gupta, S., Tenzin, T., Khan, R., Khan, T., Debnath, N., Yamage, M., Pfeiffer, D. U., & Fournie, G. (2018). A large-scale study of a poultry trading network in Bangladesh: implications for control and surveillance of avian influenza viruses. BMC veterinary research, 14(1), 12. https://doi.org/10.1186/s12917-018-1331-5
Degeling, C., Johnson, J., & Gilbert, G. L. (2019). Perspectives of Australian policy-makers on the potential benefits and risks of technologically enhanced communicable disease surveillance – a modified Delphi survey. Health research policy and systems, 17(1), 35. https://doi.org/10.1186/s12961-019-0440-3